Current issue
Archive
Online first
About the Journal
Editorial Board
Scientific Board
Reviewers
Abstracting and indexing
Publisher
Contact
Subscription
Ethical standards and procedures
Abstracting and indexing
For authors
Ethical standards and procedures
Publication charge
Books and Events
Books
Events
CASE REPORT
Closure of Full-thickness Macular Hole after Pars Plana Vitrectomy (23G) with Cataract Phacoemulsification, Artificial Intraocular Lens Implantation, and Silicone Oil Administration Due to Rhegmatogenous Retinal Detachment in the Right Eye in a 67-year-old Patient – a Case Report
1
Student Scientific Club at the Department of Ophthalmology, Department of Ophthalmology, Faculty of Medical Sciences in Katowice, Medical University of Silesia in Katowice, Poland
2
Department of Ophthalmology, Faculty of Medical Sciences in Katowice, Medical University of Silesia in Katowice, Poland
Head: Professor Dorota Wyględowska-Promieńska, MD, PhD
3
Department of Adult Ophthalmology of the University Clinical Center them. K. Gibiński Medical University of Silesia
in Katowice, Poland
Head: Professor Dorota Wyględowska-Promieńska, MD, PhD
Submission date: 2024-01-15
Acceptance date: 2024-02-19
Publication date: 2024-05-02
Ophthalmology 2024;27(1):21-23
KEYWORDS
ABSTRACT
Macular holes pose a significant threat to central vision, necessitating precise diagnosis and intervention with an occurrence of 1 per 1000 patients over the age of 55. This manuscript presents a case study of a 66-year-old man with a retinal detachment in the right eye and full-wall macular hole.
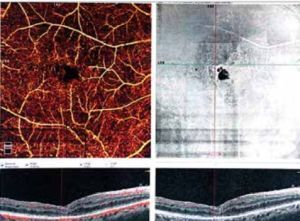
The patient underwent a multi-step surgical intervention involving pars plana vitrectomy, internal limiting membrane peeling with silicone oil tamponade, retinal endophotocoagulation, and administration and removal of the perfluorocarbon liquid DK-line in the first step. The second stage of treatment comprised silicone oil removal via posterior access vitrectomy, injection of 25% SF6 into the right eye, and treatment of intraoperatively found macular hole with an inverted flap method.
The case underscores the association between macular hole and rhegmatogenous retinal detachment, with potential iatrogenic causes during vitrectomy. The inverted internal limiting membrane flap technique emerged as a superior strategy for managing full-thickness macular holes, demonstrating high closure rates and improved visual acuity postoperatively. This case study contributes to the evolving understanding of macular hole pathogenesis and reinforces the significance of tailored surgical approaches for optimal patient outcomes.
REFERENCES (11)
1.
Macular Hole - StatPearls - NCBI Bookshelf. Accessed January 4, 2024. https://www.ncbi.nlm.nih.gov/b....
2.
GASS JD: Reappraisal of biomicroscopic classification of stages of development of a macular hole. American Journal of Ophthalmology. 1995; 119(6): 752–759. doi:10.1016/s0002-9394(14)72781-3.
3.
Duker JS, Kaiser PK, Binder S, et al.: The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and Macular Hole. Ophthalmology. 2013; 120(12): 2611–2619. doi:10.1016/j.ophtha.2013.07.042.
4.
Martins Melo I, Jhaveri A, Bansal A, et al.: Pathophysiology of secondary macular hole in Rhegmatogenous Retinal Detachment. Investigative Opthalmology & Amp; Visual Science. 2023; 64(13): 12. doi:10.1167/iovs.64.13.12.
5.
Kim DY, Jo YJ, Kim J-Y, et al.: Surgical outcomes of vitrectomy for macular hole-induced retinal detachment according to various surgical methods: A multicenter retrospective study. Seminars in Ophthalmology. 2021; 36(8): 728–733. doi:10.1080/08820538.2021.1900288.
6.
Medina CA, Ortiz AG, Relhan N, et al.: Macular Hole After Pars Plana Vitrectomy for Rhegmatogenous Retinal Detachment. Retina. 2017 Jun; 37(6): 1065–1072. doi: 10.1097/IAE.0000000000001351. PMID: 27755378; PMCID: PMC5388588.
7.
Brouzas D, Dettoraki M, Lavaris A, et al.: Postoperative eccentric macular holes after vitrectomy and internal limiting membrane peeling. International Ophthalmology. 2016; 37(3): 643–648. doi:10.1007/s10792-016-0320-6.
8.
Yuan J, Zhang L-L, Lu Y-J, et al.: Vitrectomy with internal limiting membrane peeling versus inverted internal limiting membrane flap technique for macular hole-induced retinal detachment: A systematic review of literature and meta-analysis. BMC Ophthalmology. 2017; 17(1). doi:10.1186/s12886-017-0619-8.
9.
Silva N, Ferreira A, Nawrocka (vel Michalewska) ZA, et al.: Inverted internal limiting membrane flap technique: Is it the best option for macular holes? Clinical Ophthalmology. 2021; Vol. 15: 3295–3303. doi:10.2147/opth.s284614.
10.
Michalewska Z, Michalewski J, Adelman RA, et al.: Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010; 117(10): 2018–2025. doi:10.1016/j.ophtha.2010.02.011.
11.
Yamashita T, Sakamoto T, Terasaki H, et al.: Best surgical technique and outcomes for large macular holes: Retrospective Multicentre Study in Japan. Acta Ophthalmologica. 2018; 96(8). doi:10.1111/aos.13795.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.