PRACA ORYGINALNA
Prospective Evaluation of Results of Surgical Treatment of Patients with Idiopathic Macular Hole by Phacovitrectomy and Combined Cataract and Vitrectomy Surgery
1
Department of Retina and Vitreous Surgery, Medical University of Lublin, Poland
Head: Professor Jerzy Mackiewicz, MD, PhD
Data nadesłania: 04-03-2024
Data akceptacji: 05-04-2024
Data publikacji: 02-05-2024
Ophthalmology 2024;27(1):7-14
SŁOWA KLUCZOWE
STRESZCZENIE
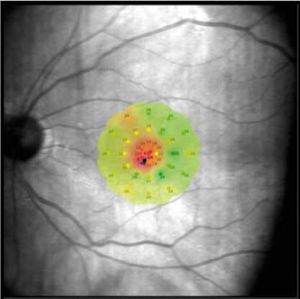
Purpose of the study:: The purpose of the study was to compare the morphological and functional results of the studied patients with idiopathic macular hole treated with a one-stage method (phacovitrectomy) and combined cataract and vitrectomy surgery. Material and methods:: The study included 33 patients (33 eyes) with idiopathic macular hole treated at the Department of Retina and Vitreous Surgery in Lublin. Twenty-one eyes were surgically treated with phacovitrectomy (Group 1 MH). Twelve patients underwent two-stage, combined treatment with removal of the lens in the first stage and vitrectomy in the second (Group 2 MH). The assignment of patients to groups was random. All patients underwent 23-gauge sutureless vitrectomy with removal of the internal limiting membrane (internal limiting membrane peeling). SF6 gas was used as an intraocular tamponade at an isovolumetric concentration of 20% and face down position recommendation for 7 days. Cataract surgery was performed using the phacoemulsification method with an incision in the transparent part of the cornea with intracapsular, posterior chamber implantation of a monofocal lens. A 12-month observation period was established, measured from the date of vitrectomy performance, and in the case of a combined procedure, this period was extended by the time between each stage of treatment. At subsequent check-ups, the subjects underwent a complete ophthalmological examination, which included: best corrected distance visual acuity and best corrected near visual acuity, assessment of the anterior and posterior segments, in a slit lamp, measurement of retinal sensitivity in the macula using microperimetry, the Amsler test and optical coherence tomography examination of the macula. Results:: In patients of the total studied group, an improvement in the best-corrected visual distance and near acuity was obtained, and in 88% retinal sensitivity in the macula was also achieved. In the group of patients subjected to phacovitrectomy (Group 1 macular hole) with an average minimum hole diameter of 487.48 µm before the procedure, after a one-year follow-up the mean best corrected distance visual acuity was 0.57 and best corrected near visual acuity 0.51, with macular retinal sensitivity of 26.65 dB. However, in the group of patients subjected to combined cataract and vitrectomy, an average minimum hole diameter of 521.58 µm 12 months after trans pars plana vitrectomy was performed as well as an average best corrected distance visual acuity of 0.64, best corrected near visual acuity of 0.5, and retinal sensitivity in the macula of 25.98 dB. There were no statistically significant differences between phacovitrectomy and the combined procedures in terms of the improvement in the values of distance and near visual acuity and macular retinal sensitivity 12 months after trans pars plana vitrectomy. A statistically significant improvement in retinal sensitivity in the macula was observed in Group 1 macular hole during the 12-month follow-up, while in the combined procedure group the improvement was not statistically significant. Conclusions:: Vitrectomy is an effective method of treating maculopathy in the form of macular hole. Morphological and functional improvement was noted in all patients, regardless of the treatment method used. There were no statistically significant differences between phacovitrectomy and the combined procedure in terms of the improvement achieved in the values of distance visual acuity parameters, near vision and retinal sensitivity in the macula 12 months after trans pars plana vitrectomy. A common feature of patients with worse results on individual variables was a longer duration of the disease and a larger size of the hole prior vitrectomy.
REFERENCJE (29)
1.
Duker JS, Kaiser PK, Binder S, et. al.: The International Vitreomacular Traction Study Classification System for Vitreomacular Adhesion, Traction, and Macular Hole. Ophthalmology. 2013; 120: 2611–2619.
2.
Wylêga³a E, Nowiñska A, Teper S: Optyczna Koherentna Tomografia II. Górnicki Wydawnictwo Medyczne, Wroc³aw 2010, s. 71–80.
3.
McCannel CA, Ensminger JL, Diehl NN, et al.: Population based incidence of macular holes. Ophthalmology. 2009; 116: 1366–1369.
4.
Wang S, Xu L, Jonas JB: Prevalence of full thickness macular holes in urban and rural adult Chinese: the Beijing Eye Study. Am J Ophthalmol. 2006; 141: 589–591.
5.
Jackson TL, Donachie PH, Sparrows JM, et al.: The United Kingdom National Ophthalmology Database study of vitreoretinal surgery: report 2, macular hole. Ophthalmology. 2013; 120(3): 629–634.
7.
Chew EY, Sperduto RD, Hiller R, et al.: Clinical course of macular holes. The Eye Disease Case-Control Study. Arch Ophthalmol. 1999; 117: 242–246.
8.
Johnson MW, van Newkirk MR, Meyer KA: Perifoveal vitreous detachment is the primary pathogenic event in idiopathic macular hole formation. Arch Ophthalmol. 2001; 119: 215–222.
9.
Gupta B, Laidlaw DA, Williamson TH, et al.: Predicting visual success in macular hole surgery. Br J Ophthalmol. 2009; 93: 1488–1491.
10.
Passemard M, Yakoubi Y, Muselier A, et al.: Long-term outcome of idiopathic macular hole surgery. Am J Ophthalmol. 2010; 149: 120–126.
11.
Kirshnan R, Tossounis C, Yang YF: 20-gauge and 23-gauge phacovitrectomy for idiopathic macular holes: comparison of complications and long-term outcomes. Eye. 2013; 27: 72–77.
12.
Michalewska Z, Michalewski J, Nawrocki J: Macular hole closure after vitrectomy: the inverted flap technique. Retina Today. 2009; 3: 73–74.
13.
Beutel J, Dahmen G, Ziegler A, et al.: Internal limiting membranê peeling with indocyanine green or trypan blue in macular hole surgery: a randomized trial. Arch Ophthalmol. 2007; 125: 326–332.
14.
Brooks HI Jr.: Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology. 2000; 107: 1939–1949.
15.
Michalewska Z, Michalewski J, Adelman RA, et al.: Inverted internal limiting membrane flap technique for large maculr holes. Ophtalmology. 2010; 107: 2018–2025.
16.
Lee JW, Kim IT: Outcomes of idiopathic macular epiretinal membrane removal with and without internal limiting membrane peeling: a comparative study. Jpn J Ophthalmol. 2010; 54(2): 129–134.
17.
Bernardos RL, Barthel LK, Meyers JR, et al.: Late-stage neuronal progenitors in the retina are radial Müller glia that function as retinal stem cells. J Neurosci. 2007; 27(26): 7028–7040.
18.
Jaycock PD, Bunce C, Xing W, et al.: Outcomes of macular hole surgery: implications for surgical management and clinical governance. Eye (Lond.) 2005; 19: 879–884.
19.
Wong SC, Clare G, Bunce C, et. al.: Cataract progression in macular hole cases: results with vitrectomy or with observation. J Cataract Refract Surg. 2012; 38: 1176–1180.
20.
Resnikoff S, Pascolini D, Etya’ale D, et al.: Global data on visual impairment in the year 2002. Bull World Health Organ. 2004; 82: 844–851.
21.
Prokofyeva E, Wegener A, Zrenner E: Cataract prevalence and prevention in Europe: a literature review. Acta Ophthalmol. 2013; 91(5): 395–405.
22.
Ghosh S, Best K, Steel DH: Lens-iris diaphragm retropulsion syndrome during phacoemulsification in vitrectomized eyes. J Cataract Refract Surg. 2013; 39: 1852–1858.
23.
Lee JY, Kim KH, Shin KH, et al.: Comparision of intraoperative complications of phacoemulsification between sequential and combined procedures of pars plana vitrectomy and cataract surgery. Retina 2012; 32: 2026– –2033.
24.
Rejdak R: Wskazania do witrektomii. Via Medica, Gdañsk 2017, s. 67. ISBN 978-83-65797-07-0.
25.
Scartozzi R, Bessa AS, Gupta OP, et al.: Intraoperative sclerotomy-related retinal breaks for macular surgery, 20-versus 25-gauge vitrectomy systems. Am J Ophthalmol. 2007; 143: 155–156.
26.
Muselier A, Dugas B, Burelle X, et al.: Macular hole surgery and cataract extraction: Combined vs consecutive surgery. Am J Ophthalmol. 2010; 150: 387–391.
27.
Krishnan R, Tossounis C, Yang YF: 20-gauge and 23-gauge phacovitrectomy for idiopathic macular holes: comparison of complications and long-term outcomes. Eye. 2013; 27: 72–77.
28.
Ruiz-Moreno JM, Arias L, Araiz J, et al.: Spectral-domain optical coherence tomography study of macular stucture as prognostic and determining factor for macular hole surgery outcome. Retina. 2013; 33: 1117–1122.
29.
Michalewska Z, Michalewski J, Nawrocki J: Diagnosis and evaluation of macular hole with the HRT 2 retina module. Ophthalmologe. 2007; 104: 881–888.
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.